Injuries
Our physiotherapists undergo rigorous training to ensure that you receive top-notch treatment and care.
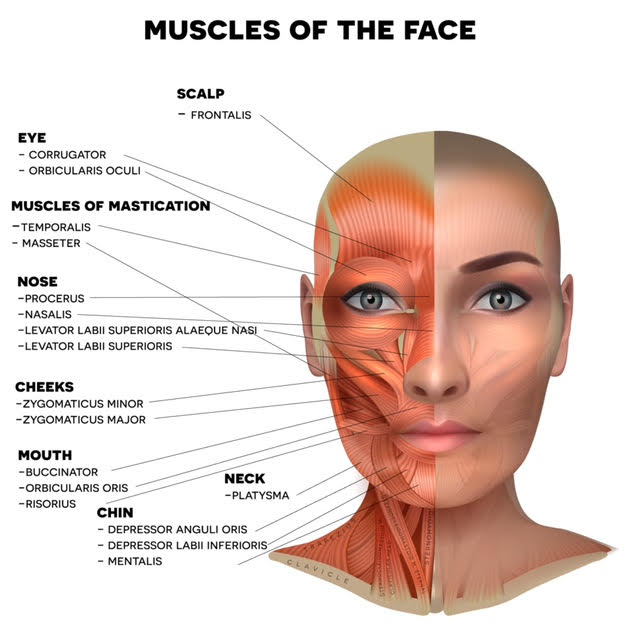
Physical Therapy Guide to Bell’s Palsy: Understanding Facial Paralysis
Bell’s palsy is a temporary condition that affects facial movements and can have a significant impact on daily life. It occurs when the facial nerve becomes inflamed, resulting in sudden weakness or paralysis on one side of the face. It’s important to note that these symptoms can sometimes be signs of a severe condition like a stroke.
If you experience any facial weakness, seek immediate medical attention. Call an ambulance if you also experience ear, cheek, or teeth pain, loss of facial sensation, confusion, weakness in arms or legs, vision changes, fever, or a headache.
Physical therapists are experts in movement and can help improve your quality of life. They provide hands-on care, educate patients, and offer tailored exercises to enhance movement and recovery. If you suspect Bell’s palsy or experience facial weakness, consider contacting a physical therapist for an evaluation.
TMJ dysfunction (TMD)
The temporomandibular joint (TMJ), which functions like a sliding hinge, connects your jawbone to your skull. You have one TMJ on each side of your jaw. TMJ disorders, a subset of temporomandibular disorders (TMD), can lead to pain in the jaw joint and the muscles responsible for jaw movement.
Determining the exact cause of TMJ disorders can be challenging. It’s often the result of a combination of factors, such as genetics, arthritis, or jaw injuries. Some individuals who experience jaw pain may also have a tendency to clench or grind their teeth (bruxism). However, it’s important to note that many people grind or clench their teeth habitually without developing TMJ disorders.

Fortunately, in most cases, the pain and discomfort associated with TMJ disorders are temporary and can be managed with self-care or non-surgical treatments. Surgery is typically considered a last resort when conservative approaches have not provided relief. Nonetheless, some individuals with TMJ disorders may find surgical treatments beneficial.
Back pain, especially that troublesome lower back pain, is one of the most familiar issues people bring to the physiotherapy clinic. The good news is, in many cases, it can be managed effectively, and the pain usually eases up within a few days to a few weeks.

Back pain is often a short-lived problem, lasting for a few days or a few weeks. It’s frequently linked to everyday movements, like lifting heavy objects, spending too long gardening, or even sitting for extended periods. Physiotherapy can be your ally in reducing that discomfort and helping you regain your freedom of movement.
Common Back Problems:
-
Disc Injuries: The discs in your lower back are like load-bearing cushions. Sometimes, they can get damaged due to excessive bending or sudden trauma, leading to back pain and occasionally leg pain (often known as “sciatic pain”) and other nerve-related symptoms in your legs.
-
Ligament/Facet Joint Sprains and Muscle Spasms: These issues often occur after heavy lifting, prolonged bending, or sports-related injuries. The joints in your lower back can get overstretched, and the muscles around your spine may tighten and go into spasm mode to shield your back.
-
Postural Back Pain: Believe it or not, poor posture is a major culprit for back pain. Factors like how you sleep, your workstation setup, and the way you stand or sit can contribute to this type of discomfort. Patients dealing with postural back pain often need to address muscle imbalances and work on enhancing their core stability.
-
Degenerative Changes: Over time, the joints and discs in your spine may start showing signs of wear and tear. These changes usually happen gradually and can be aggravated if you spend long hours standing.

Back Pain Treatment: When you come in for a physiotherapy assessment for your back pain, we can determine the underlying causes and tailor a treatment program to suit your goals. Treatment may involve techniques like joint mobilization, massage, dry needling, taping, stretches, postural adjustments, and ergonomic advice. For those with back injuries, rehabilitation often includes an exercise regimen designed to strengthen core and postural muscles, as well as improve flexibility.
Neck pain is a frequent issue that we encounter in our clinic. Typically, this discomfort is caused by various factors within or around the head and neck, or it might be referred pain from other sources like the upper back, jaw, or shoulders.
Headaches, which are described as pain in the head, around the eyes, ears, or the back of the head, come in many different forms and have various causes. The most common type of headache that physiotherapists treat is known as a cervicogenic (or tension) headache.

Common Neck Injuries:
Postural Neck Pain: Poor posture often plays a starring role in neck pain. Things like your sleeping position, workstation setup, and how you sit can contribute to this discomfort. Typically, folks with postural neck pain and neck stiffness need to address muscle imbalances, especially tightness in their neck and chest muscles and weakness in the stabilizing muscles of the neck, upper back, and shoulders. Treatment for neck pain may involve soft tissue and joint mobilization of the cervical and thoracic spine.
Bulging or Protruding Disc: The discs in your spine have a jelly-like interior (nucleus pulposus) that can change shape and distribute load as your spine moves. Surrounding this is strong connective tissue (annulus fibrosus) designed to maintain the disc’s normal shape. A disc bulge happens when the nucleus pulposus swells out of shape due to tears or damage in the annulus fibrosus. This can put pressure on spinal nerves, causing symptoms like neck pain, headaches, arm pain, tingling, and possible numbness. Physiotherapy treatment, involving a mix of ‘hands-on’ therapy and exercise-based rehabilitation, is typically effective.
Acute Wry Neck: This is characterized by neck and upper back pain due to damage and ‘locking’ of a facet joint in the neck. It results in limited movement range and a posture where your neck is typically fixed or tilted to one side. Trying to move from this position usually leads to sharp pain. It can result from sudden neck movements or heavy lifting. Early intervention with physiotherapy often resolves symptoms within a few days.
Cervicogenic (Tension) Headaches: These headaches often originate at the back of the head and upper neck, presenting as a tight band or pressure. They can have various pain patterns, from a ‘headband’ sensation to a sharp, throbbing pain behind the eyes. These headaches can be one-sided or affect both sides, varying in intensity and are sometimes mistaken for migraine. They may even cause dizziness and nausea. Prolonged sitting or poor posture can aggravate them. Fortunately, physiotherapy is typically highly effective in managing these headaches, and your physiotherapist may also offer advice on posture.
Whiplash: Whiplash is an injury to the neck resulting from a rapid forward and backward motion of the head, often due to car accidents, falls, or sports tackles. It can lead to increased neck pain and stiffness. If left untreated, it may become a chronic and debilitating issue. Early advice and intervention are recommended.

The shoulder joint is quite a remarkable assembly, consisting of three key bones: the upper arm bone (humerus), shoulder blade (scapula), and collarbone (clavicle). Adding to this intricate structure are the crucial rotator cuff muscles that encircle the shoulder, helping to keep it steady. To ensure smooth movement, there’s a handy lubricating sac called a bursa positioned between the rotator cuff and the bony ridge on your scapula, which rests atop your shoulder, known as the acromion.
What makes the shoulder fascinating is its exceptional mobility, granting it a broader range of motion compared to other joints in your body. However, this flexibility comes at a cost, as it’s more susceptible to instability, making it a frequent site for injuries.

Common Shoulder Injuries:
- Shoulder Impingement: Imagine your rotator cuff tendon and bursa getting pinched or wedged between the acromion and the head of your humerus. This can occur when you reach your arm over your shoulder or rotate it inward. It results in inflammation, restricting your shoulder’s movement and causing pain. Symptoms include pain at the front or top of your shoulder, sometimes radiating down your arm, especially when lifting heavy objects or reaching above shoulder height. You might also experience discomfort when lying on the affected shoulder.
Shoulder impingement can be triggered by various factors like shoulder trauma, repetitive reaching or prolonged mouse use, poor posture, and abnormal biomechanics. A shoulder physiotherapist can help identify the root cause, alleviate the pain, and enhance your mobility. Typically, physiotherapy combined with specific exercises effectively addresses shoulder impingement. In some cases, when physiotherapy isn’t sufficient, a cortisone injection may be considered.
-
Rotator Cuff Tears: The rotator cuff comprises four muscles, and tears can affect one or more of these muscles or their tendons. Such tears may result from a sudden injury, such as a fall or heavy lifting, or develop gradually due to tendon overuse. Spontaneous tears, often seen in patients over 60 or those who’ve taken high doses of steroid medications for extended periods, can cause pain at the front or top of the shoulder, occasionally radiating down the arm. Range of motion may be limited and painful, especially when reaching forward or to the side. Strength in the shoulder may also decrease, depending on the tear’s severity. Minor tears can usually be managed conservatively with physiotherapy and exercise rehabilitation, but more severe tears may require surgery.
-
Referred Pain: Shoulder pain is not always a local issue; it can sometimes originate from other areas, like the neck or upper back. This may lead to pain around the back of the shoulder and upper arm, occasionally extending to the forearm, wrist, and hand, and possibly accompanied by pins and needles or numbness. A thorough assessment by your physiotherapist will help pinpoint the source of your shoulder pain, allowing them to create a suitable treatment plan.

At Auburn Physiotherapy, we’re dedicated to providing you with a specialized shoulder physiotherapist in Sydney who will support and track your recovery progress.
What’s the Deal with Elbow Pain?
Elbow pain can be a real bother, and it usually strikes in one of two spots: on the outside, known as tennis elbow or extensor tendinopathy, or on the inside, which is called golfer’s elbow or flexor tendinopathy. Don’t be misled by the names; you don’t need to be a sports enthusiast to experience these aches!
Both golfer’s and tennis elbow are essentially tendon injuries, where the muscles connect to the bone. These injuries often result from a gradual overuse of the tendon. Everyday activities, like typing on a computer, or overdoing it in sports, can lead to these issues. Interestingly, most elbow pain originates from higher up in the upper back, neck, or shoulder, which can place extra stress on the elbow. This can cause discomfort and weakness in wrist and hand movements.

So, How Do You Treat It?
Elbow pain is commonly managed with a combination of ice, a bit of rest from the activities that really aggravate it, and exercises to promote tendon healing. In some cases, your physiotherapist may also recommend techniques like dry needling and soft tissue release for the forearm, shoulder, and neck. It’s crucial to remember that while it might hurt, this condition is usually not something to worry about, and using your arm throughout the day can actually help with the healing process. Taking full rest often makes the tendon problem worse and prolongs recovery. Additionally, addressing the underlying causes of the elbow pain can speed up the healing process.

How Long Does It Take to Get Better?
Tendons are rather slow to mend, and it might take anywhere from 8 to 12 weeks for a complete resolution with the right treatment. However, the good news is that most of the pain should subside well before that. Your physiotherapist can provide you with a more precise prognosis based on your specific diagnosis.
If you’re grappling with elbow pain, don’t hesitate to get in touch with Auburn Physiotherapy today!
Demystifying Hand and Wrist Pain
Your hand and wrist are quite the intricate system, made up of around 29 bones (some people even have 30!), supported by over 120 ligaments. Keeping this machinery moving are approximately 34 muscles, some tucked in your hand and others in your forearm. Fun fact: there are no actual muscles in your fingers; it’s all about tendons!
Now, here’s the kicker: any of these structures can get injured or cause you pain. This can range from fractures and ligament sprains to muscular and tendon strains, not to mention overuse issues like repetitive strain injuries.

So, How Do We Figure It Out?
When it comes to pinpointing the source of your discomfort, we kick things off by delving into your symptoms. We want to know how long you’ve been experiencing the pain, what makes it worse, and if there’s anything that eases your suffering.
Next, we take a closer look at how your fingers, hand, and wrist are moving. Physios have a bunch of nifty tests up their sleeves to help identify the culprit behind your pain.
But that’s not all! We also consider how your entire arm and body are functioning because sometimes, issues in your hand and wrist can be traced back to what’s happening at your shoulder, neck, or back.
So, What’s the Game Plan?
Treatment for acute muscle strains usually involves exercises that help with stretching and strengthening. Chronic injuries, such as repetitive strain injuries, can be a bit more complex and may call for techniques like soft tissue releases and dry needling, combined with exercises to ease the affected area.
For ligament injuries, the focus is on stabilizing the affected joint or joints to prevent further sprains and facilitate healing.
Fractures are handled by stabilizing the injured area to reduce strain on the affected bone, alleviate pain, and support proper healing and function. This may involve using a splint, brace, or cast.
What’s the Light at the End of the Tunnel?
As a general rule, the duration and intensity of your pain play a role in determining how quickly you’ll recover from muscular and tendon strains. Ligament sprains can take between 6 to 12 weeks to heal, depending on which ligament is affected and the seriousness of the injury.

Fractures of the hand and wrist typically take 6 to 12 weeks to mend. After the fracture has healed, you may experience a period of stiffness, weakness, and reduced control of your hand and wrist. Getting back to full strength may take several more weeks.
If you’re grappling with hand and wrist pain, stiffness, or discomfort, don’t hesitate to pay us a visit in the Auburn Physiotherapy clinic today!
Demystifying Hand and Wrist Pain
Your hand and wrist are quite the intricate system, made up of around 29 bones (some people even have 30!), supported by over 120 ligaments. Keeping this machinery moving are approximately 34 muscles, some tucked in your hand and others in your forearm. Fun fact: there are no actual muscles in your fingers; it’s all about tendons!
Now, here’s the kicker: any of these structures can get injured or cause you pain. This can range from fractures and ligament sprains to muscular and tendon strains, not to mention overuse issues like repetitive strain injuries.

So, How Do We Figure It Out?
When it comes to pinpointing the source of your discomfort, we kick things off by delving into your symptoms. We want to know how long you’ve been experiencing the pain, what makes it worse, and if there’s anything that eases your suffering.
Next, we take a closer look at how your fingers, hand, and wrist are moving. Physios have a bunch of nifty tests up their sleeves to help identify the culprit behind your pain.
But that’s not all! We also consider how your entire arm and body are functioning because sometimes, issues in your hand and wrist can be traced back to what’s happening at your shoulder, neck, or back.
So, What’s the Game Plan?
Treatment for acute muscle strains usually involves exercises that help with stretching and strengthening. Chronic injuries, such as repetitive strain injuries, can be a bit more complex and may call for techniques like soft tissue releases and dry needling, combined with exercises to ease the affected area.
For ligament injuries, the focus is on stabilizing the affected joint or joints to prevent further sprains and facilitate healing.
Fractures are handled by stabilizing the injured area to reduce strain on the affected bone, alleviate pain, and support proper healing and function. This may involve using a splint, brace, or cast.
What’s the Light at the End of the Tunnel?
As a general rule, the duration and intensity of your pain play a role in determining how quickly you’ll recover from muscular and tendon strains. Ligament sprains can take between 6 to 12 weeks to heal, depending on which ligament is affected and the seriousness of the injury.

Fractures of the hand and wrist typically take 6 to 12 weeks to mend. After the fracture has healed, you may experience a period of stiffness, weakness, and reduced control of your hand and wrist. Getting back to full strength may take several more weeks.
If you’re grappling with hand and wrist pain, stiffness, or discomfort, don’t hesitate to pay us a visit in the clinic today!
Cracking the Code of Knee Pain
Knee pain is like a puzzle, with various pieces that can contribute to the discomfort. These pieces include muscles, tendons, ligaments, and the all-important cartilage (known as the meniscus). Surprisingly, knee pain isn’t always a local issue; it can also be referred from other areas, like your lower back or hip. Injuries to the knee can occur gradually over time or suddenly due to trauma.
Sudden knee injuries often happen to athletes in sports that involve quick changes of direction, twisting, and kicking – think football, soccer, basketball, netball, or skiing. These injuries often involve tearing of the meniscus (that vital cartilage) or knee ligaments.
Gradual-onset knee pain is typically the story for those who engage in activities with lots of running, repetitive squatting, lunging, jumping, twisting, kneeling, or repetitive kicking. One of the frequent culprits behind front-of-the-knee pain is patellofemoral pain syndrome. This condition often arises from biomechanical problems or muscle imbalances, causing the kneecap to veer off track. Over time, this can irritate the surrounding soft tissues. If left untreated, the symptoms tend to worsen and might limit your ability to participate in sports or activities.
Common knee injuries include:
- ACL Injury
- Patellofemoral Pain
- Meniscal or Cartilage Injuries
- Iliotibial Band Friction Syndrome
- Patella Tendinopathy

Your trusty physiotherapist is here to decipher the knee pain enigma. They’ll assess your knee and provide a diagnosis and treatment plan. This often involves techniques like soft tissue release, dry needling, and addressing underlying issues, including weaknesses in the foot and hip. They’ll also prescribe an exercise program to get you back on your feet as swiftly as possible.
If you find yourself wrestling with knee pain, don’t hesitate to visit Auburn Physiotherapy today. We’re here to help you crack the code and pave the way to relief.
When it comes to sports injuries, you want the best care available. That’s where sports injury physiotherapists step in, offering you a range of essential services to get you back in the game:
- Same-Day Appointments: We understand the urgency, so we’re here when you need us.
- One-on-One Treatment: Your recovery is our sole focus during every session.
- Convenient CBD Location: We’re right where you need us, in the heart of the city.
- Claim on the Spot: We’ve got the paperwork sorted so you can concentrate on healing.
- Full Assessment and Accurate Diagnosis: We leave no stone unturned to uncover the root of the issue.
- Treatment of the Cause, Not Just the Symptoms: Our goal is to ensure long-lasting recovery.
- Hands-On Treatment and Expert Advice: We provide manual therapy and guide you with tailored strengthening and stretching exercises.
- Referral to Specialists if Required: If your case requires extra expertise, we’ve got you covered.

Ankle Sprain: The most common ankle injury is the dreaded inversion sprain, often referred to as a “rolled ankle.” It involves stretching or tearing the ligaments, typically the lateral ones on the outside of the ankle. Sometimes, it can also damage the tendons beneath the lateral malleolus (the lateral ankle bone). Treatment encompasses the RICE method (rest, ice, compression, elevation) along with manual therapy to restore normal ankle function. Strengthening exercises and proprioception work are crucial to rebuild strength and stability and reduce the risk of recurrence.
Ankle Fracture: Ankle fractures can mimic ankle sprains, making it vital for your physiotherapist to differentiate between the two. They’ll send you for an x-ray if they suspect a fracture. Treatment for fractures typically involves immobilizing the ankle in a boot or cast for about 4-6 weeks.
Achilles Injuries: Achilles injuries can manifest as tendinopathy or a complete rupture. Tendinopathy is usually an overuse injury linked to biomechanical problems, muscle imbalances, training intensity, or unsuitable footwear. Physiotherapy plays a crucial role in managing tendinopathy by addressing biomechanical and training issues. Achilles tendon rupture, on the other hand, is an acute injury where the tendon fibers partially or completely rupture. Management can be conservative with physiotherapy and immobilization in a boot or surgical, depending on the severity.
Plantar Fasciitis: Plantar fasciitis leads to pain under your foot near the heel. It often strikes in the morning or after prolonged sitting, and it can intensify with walking or running. Biomechanical issues related to foot alignment are commonly to blame. Typically, physiotherapy treatments can effectively manage it, but in some cases, you might need a referral to a podiatrist.

Stress Fracture: Stress fractures are like small cracks in the bone. In the foot, they’re often seen in the metatarsal bones. Weight-bearing activities, such as running, can put excessive or repetitive loads on the bones, causing gradual damage and leading to a stress fracture. Diagnosis may require scans. Initial treatment involves immobilization in a boot, followed by physiotherapy to restore range of motion and strength.
So, if you’re dealing with a sports injury, don’t hesitate to reach out to us. We’re here to help you recover, regain your strength, and get back to doing what you love.
Navigating the World of Sports Injuries
Sports injuries are a familiar part of the sporting realm, ranging from the occasional sprained ankle to the more severe dislocated shoulder. Our dedicated team at Auburn Physiotherapy is here to guide you through this challenging terrain. We’ll meticulously assess your injury, provide a diagnosis, and map out a treatment plan to fast-track your return to the field.

These injuries can sprout from various sources, such as:
Overtraining: When you push yourself too hard, it can lead to overuse injuries like tendinopathies or muscle tears.
Undertraining: Conversely, not preparing your body adequately for the activity can put excessive stress on unconditioned tissues.
Incorrect Equipment: The wrong gear or footwear can spell trouble, causing issues from foot and ankle pain to hip and even back pain.
Biomechanics and Technique: Poor running technique can contribute to overuse injuries, including the notorious runner’s knee.
Accidents: Sometimes, gravity is not your friend. Falls and collisions can result in sprains and contusions (those painful bruises).
Auburn Physiotherapy excels at uncovering the root causes that may have led to your sports injury, helping to prevent its recurrence. If you do happen to sustain a sports injury, it’s crucial to seek assessment and treatment from a sports injury physiotherapist during the acute phase (the first 48 to 72 hours). This early intervention enables the physiotherapist to precisely diagnose the injury and devise a treatment plan to expedite your return to the game.
Here are some common sporting injuries we can assist with:
- Achilles Tendinopathy
- Ankle Sprain
- Plantar Fasciitis
- Calf Strain or Tear
- Shin Pain
- ACL Injury
- Patella-Femoral Pain
- Meniscal or Cartilage Injuries of the Knee
- Iliotibial Band Friction Syndrome
- Patella Tendinopathy
- Hamstring Strain or Tear
- Hip and Groin Injuries
- Sports Hernia
- Tennis Elbow and Golfer’s Elbow
- Shoulder Dislocation
- Rotator Cuff Injuries and Tears
- Shoulder Impingement
- Running Injuries

If you find yourself facing an injury that demands immediate attention, don’t hesitate to reach out to Auburn Physiotherapy now at 02 96464656 to schedule your Sydney sports physio appointment. We’re here to get you back in the game swiftly and safely.
Understanding Running Injuries
Running injuries, as the name suggests, are injuries that occur while running or as a result of running. They can manifest in various parts of your body, from your feet and knees to your hips, back, or even your neck. It’s worth noting that these injuries are not exclusive to running and can stem from any form of exercise or sports activity. Some of the more common running-related injuries include:

- Achilles Tendinopathy
- Plantar Fasciitis
- Calf Strain or Tear
- Shin Pain
- Patella-Femoral Pain
- Iliotibial Band Friction Syndrome
- Patella Tendinopathy
Diagnosis: To pinpoint the cause of your discomfort, our physiotherapists adopt a holistic approach. We start by assessing the area of your body that’s causing you the most pain, but we also extend our examination to your entire body. This includes scrutinizing your running technique on a treadmill to gain a comprehensive understanding.
Treatment: The treatment plan hinges on the diagnosis. Once we’re certain about the underlying cause of your pain, we have a range of techniques at our disposal to kickstart the rehabilitation process. As the saying goes, there’s more than one way to solve a problem.
One effective approach for addressing running injuries is by refining your running form. There are various running styles and techniques to accommodate different body types, and we’ll help you develop a running style that suits your body and movement patterns.
Additional treatment techniques encompass mobilizations, soft tissue releases, dry needling, and exercises tailored to help you stretch, strengthen, and control the relevant structures, among others.
Prognosis: The outlook for recovery varies depending on the specific injury. In general, the shorter the duration of the injury and the milder the pain, the quicker the recovery.

If you’re grappling with running-related injuries, don’t hesitate to pay us a visit at the clinic today. We’re here to help you on your path to recovery.
Embarking on the Road to Post-Operative Recovery
Post-operative rehabilitation, as the name implies, is the process of recuperation following surgery. You may have heard of various surgeries like ACL reconstructions, rotator cuff repairs, ankle, knee, and hip arthroscopies, shoulder reconstructions, and cervical and lumbar discectomies and fusions. These are just a few examples of surgeries that can necessitate post-operative rehabilitation.

Diagnosis: In the realm of post-surgery, there’s not much to diagnose, as the condition and the surgery performed are typically known. However, at Auburn Physiotherapy, we take a comprehensive approach. We assess and diagnose any other injuries, abnormalities, or imbalances in your body that could influence your rehabilitation and recovery from surgery. This assessment can occur both before and after surgery. It provides a head start on your recovery or potentially even delays the need for surgery if the condition is minor.
Treatment: Physiotherapists employ various tools to optimize your recovery. One common approach involves teaching you exercises that help restore strength, range of motion, and function that may have been compromised by your injury and surgery. At Auburn Physiotherapy, we use an online exercise program called TrackActive. Through TrackActive, our physios provide exercises via email. You’ll have access to pictures, videos, and clear instructions, ensuring you perform exercises correctly. TrackActive also offers a recording system that allows you and your physio to monitor your progress. It’s a valuable way to receive day-to-day feedback between your physio sessions in the clinic.

Prognosis: Recovery time frames hinge on the specific surgery and the instructions provided by the surgeon. Your goals, whether it’s a return to exercise, sports, or daily life activities, can also influence the duration of your recovery.
If you have surgery scheduled or it’s been recommended, why not pay us a visit at the clinic today and kickstart your rehabilitation journey? We’re here to guide you on the path to a successful recovery.
Understanding Cervicogenic Headaches
Headaches, characterized by pain in the head, around the eyes or ears, and often radiating to the back of the head, come in various types and stem from diverse causes. Among these, cervicogenic headaches are a common concern addressed by physiotherapists.

What’s a Cervicogenic Headache Like?
Cervicogenic headaches typically manifest as a tight band-like sensation or pressure at the back of the head and upper neck. The pain can assume different patterns, such as resembling a headband of discomfort or a sharp throbbing sensation behind the eyes. These headaches can affect one or both sides of the head, range from mild to severe in intensity, and might be mistaken for migraines without aura. Some individuals may even experience dizziness and nausea. Certain postures or positions, like prolonged computer use, can exacerbate these headaches. Neck and upper back stiffness often contribute to their development. The good news is that cervicogenic headaches usually respond exceptionally well to physiotherapy. Your physiotherapist can provide postural and ergonomic advice if these factors are contributing. They may also discuss proper pillow and workstation setups and offer other preventive measures.
How Are They Treated?
Your physiotherapist will delve into the underlying causes of your headaches. Treatment typically includes soft tissue release and joint mobilization in the upper neck, back, and shoulders. They’ll equip you with exercises designed to alleviate headaches and maintain the mobility of your neck and back.
If you’re grappling with headaches, reach out to Auburn Physiotherapy for effective treatment and relief.
CLINIC LOCATIONS
Auburn Physiotherapy & Allied Health Clinic: Suit 304, 39 queen st, Auburn, NSW, Aus
Phone: 02 96464656
Mail Us: auburnphysiotherapy@gmail.com
Auburn Physiotherapy – CENTRAL for REHAB PHYSIOTHERAPY offers a comprehensive range of healthcare services designed to meet your diverse needs.
